The CDC mask experiment studies quick sheet.
Because its been 3 years and you still haven't read the actual science.
If you use a butter knife to cut and spread butter, will it work? Well it seems like it would.
What about using a butter knife to cut a broomstick? Hmmm not sure.
But we can actually test the knife out by slicing through butter. Yep it “slices”, just like knives are built to do, so yes it will slice through a broom handle.
You see, that's how the CDC mask science works. They showed masks doing the one trick they know how to do, and in the best possible set up to do it, with the shortest amount of time to have “show off” doing it.
The general public doesn’t realize this, but NO NEW information about masks was discovered in the new Covid mask science. Almost all of the experiments were nothing more than rehashed copies of older experiments.
The fun part of this article is when you get to the end and you realize that the butter knife analogy is exquisitely accurate.
bon appétit. Enjoy the brain nourishment.
In the construction of this article, a priority is to give sufficient sampling of information, while keeping overall length from it becoming an entire book.
My goal here is to peak your interest and motivate you to actually read ALL of the studies THOROUGHLY.
I suspect that these studies were chosen by the CDC because of the good filtration numbers the tests produced. At a glance the masks look good on paper. These studies also use positive affirming language in their conclusions and discussions. It is clear that the authors themselves believe in masks.
...but...when you put your glasses on and comb through the lines, there are important things to be found.
Things that alter the meaning of the numbers and the good words.
You will find that, aside from the occasional “mention” of some real world factors. Not a single study explores them as part of the actual work. These studies are all early building block level studies ( many of them even acknowledge this themselves), yet, they are being used as the backbone of public policy. Even worse they are the often referenced as irrefutable “proof”.
Ok lets dive in
My criteria for choosing excerpts is to;
A) Show that there does exist in the body of work, authors observations and results that do not support the theory of source control
B) Do not support the theory that masks work in this new situation outside of the lab called 'universal public masking”.
C) Comments that I was surprised even exist in studies that drive pubic policy, considering all that we were told by doctors and authorities.
The studies below are numbered according to their position on the CDC 90 study list.
Bold emphasis within excerpts are mine to highlight an important point, but this doesn’t mean ignore the rest of the paragraph. I’ve included the text to give you a more robust understanding.
I know its long, technical and boring….but now isn’t the time to be lazy and just assume the people in authority know what they’re talking about.
It will become clear as day to you that not a single one of them ever actually read the science.
If you are an Industrial Hygienist, and care anything about the integrity of your Exposure Sciences…then YOU especially, need to pay attention to what you are about to read.
Mask Experiment Studies
(#3) Efficacy of face masks, neck gaiters and face shields for reducing the expulsion of simulated cough-generated aerosols
Funding: CDC
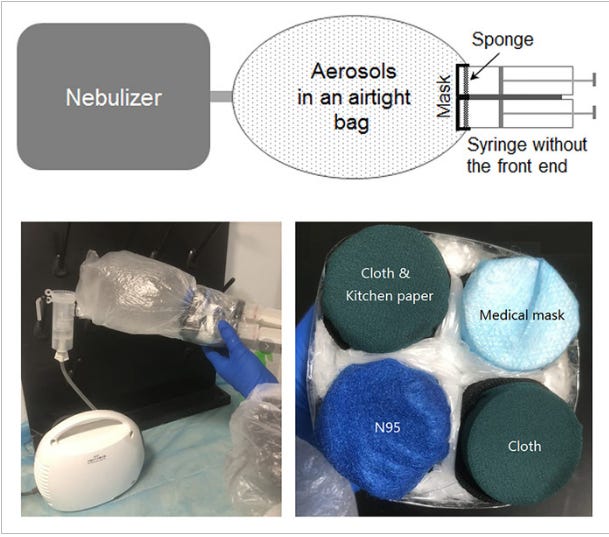
Experiment Description: Mechanical manikin head in a sealed tube chamber, wearing mask. A single cough was expelled, then after 20 minutes time to let droplets finish trajectory, mask surface and chamber surfaces were measured to calculate amount the mask stopped. That whole process was repeated 6 times.
It might be noteworthy that the head and sealed tube were vertical rather than horizontal. The cough was in a downward motion. This might cause more particles stay in or on the mask surface rather than in some way be influenced by gravity. For example, dropping away from collecting on the outside surface of the mask.
Some noteworthy excerpts;
“Small aerosols require much higher air velocities to deposit by impaction than do larger aerosols, and thus are more difficult to block with source control devices (Hinds 1999; Lindsley 2016).”
“but as with all personal protection and source control devices, their limitations must be respected.”
Unfortunately, the use of face masks and other face coverings by the general public can present challenges. People often dislike wearing masks, and compliance can be low and inconsistent (Longtin et al. 2009). Mask wearers may repeatedly don, doff and adjust face masks, which can contaminate the hands and potentially lead to disease transmission, especially when the masks are reused (Brady et al. 2017; Casanova et al. 2008). For cloth masks, the filtration efficiency and air flow resistance of different textiles varies widely (Konda et al. 2020; Teesing et al. 2020; Wilson et al. 2020). Alternative face coverings such as neck gaiters (an elastic fabric tube that fits snugly around the head and neck) are commonly used, but information about their performance as source control devices is limited. Factors such as how well the mask fits the face and the coverage provided by a mask can have a substantial impact on the effectiveness of face masks (Davies et al. 2013; Lawrence et al. 2006). Comparisons of face coverings have found substantial differences in the ability of different types of these devices to reduce the release of respiratory aerosols (Asadi et al. 2020; Davies et al. 2013).
A look at some of the paragraphs references:
Brady et. Al 2017 - “The average MS2 transfer from filtering facepiece respirators to the subjects' hands ranged from 7.6–15.4%”...”The findings suggest that the results of fluorescein and MS2 transfer were consistent and highly correlated across the conditions of study. The data supports CDC recommendations for using proper doffing techniques and discarding filtering facepiece respirators that are directly contaminated with secretions from a cough or sneeze.”
Casanova et.al. - “Although PPE is usually worn only for short periods, viruses such as influenza (10) and SARS coronavirus (11) can survive for hours on surfaces, and viral infection can be spread by surface-to-hand (12) and hand-to-hand contact (13).”
Konda et.al. 2020 - “the tests carried out with the 1% opening surprisingly resulted in significant drops in the mask efficiencies across the entire size range (60% drop in the >300 nm range)” [ note: covid is even smaller at 140nm]
Teesing et.al. 2020 – This was a predictive model based study concluding that covid spread would be reduced to 1% if 39% of the population wore a specific mask. However the model is based on filtration math only. No length of time given, no human error considered.
Wilson et.al.2020 - “Limitations include not accounting for viral transfer from the hands to the mask during mask adjustments, and assuming that all masks were worn in the same way.”
Davies et.al 2013 - “Although any material may provide a physical barrier to an infection, if as a mask it does not fit well around the nose and mouth, or the material freely allows infectious aerosols to pass through it, then it will be of no benefit.”
Lawrence et. al. 2006 – This study was about demonstrating that “fit testing” in hospital settings, improved overall PPE performance. Not about whether masks work.
Asadi et.al. 2020 - “rubbing mask fabrics generates a considerable number of particles in the range of 0.3–5 µm similar to that observed for the expiratory activities. This finding corroborates the interpretation that some proportion of the particulates observed during expiration were particulates aerosolized from the masks themselves.” [note: This study was ignored by the CDC, but Asadi's other study with a camera showing that talking produces droplets, was included in their lineup (CDC #11)]
(#4) Low-cost measurement of face mask efficacy for filtering expelled droplets during speech
Funding: grant number 2019-198099 from the Chan Zuckerberg Initiative DAF and Duke University
Experiment Description: Various common masks tested. An operator wears a face mask and speaks into the direction of an expanded laser beam inside a dark enclosure. Droplets that propagate through the laser beam scatter light, which is recorded with a cell phone camera. A video of approximately 40 s length to record droplets emitted while speaking. The first 10 s of the video serve as baseline. In the next 10 s, the mask wearer repeated the sentence “Stay healthy, people” five times (speech), after which the camera continued to record for an additional 20 s (observation). For each mask and for the control trial, this protocol was repeated 10 times.
Some noteworthy excerpts;
“We noticed that speaking through some masks (particularly the neck gaiter) seemed to disperse the largest droplets into a multitude of smaller droplets (see fig. S5), which explains the apparent increase in droplet count relative to no mask in that case”
“A first limitation is that our experimental implementation samples only a small part of the enclosure, and hence, some droplets that are transmitted through the masks might not be registered in the laser beam.”
“Second, the use of a cell phone camera poses certain limitations on detection sensitivity, i.e., the smallest recognizable droplet size.”
(#5) Visualizing the effectiveness of face masks in obstructing respiratory jets
Funding: Not declared; but likely Department of Ocean and Mechanical Engineering, Florida Atlantic University
Experiment Description: Mechanical mannequin head mounted at adult height and configured to expel equivalent droplets from a single cough or sneeze. A fog machine and lazer beam were used to highlight droplets interaction with air in front of the mask. Time and distance, including past 6 ft. forward were measured after each single cough.
Some noteworthy excerpts;
“We note that it is likely that healthcare professionals trained properly in the use of high-quality fitted masks will not experience leakage to the extent that we have observed in this study. However, leakage remains a likely issue for members of the general public who often rely on loose-fitting homemade masks. Additionally, the masks may get saturated after prolonged use, which might also influence their filtration capability. We reiterate that although the non-medical masks tested in this study experienced varying degrees of flow leakage, they are likely to be effective in stopping larger respiratory droplets.”
Three observations about that paragraph; “trained properly in use”..is a direct acknowledgment to the behavior mechanic of a masks function. ( Which I cover extensively over here) Next, “masks may get saturated after prolonged use...” Yes, they are identifying a real world parameter that exists in Universal Public Masking...ok guys then why didn't you include this step in your experiment. These real world questions are exactly what you are supposed to be answering. Lastly, “experienced varying degrees of flow leakage....”...that sentence is a complete assumption of real world results, based on one cough. We need real world results from real world parameters...multiple coughs, sneezes, and constant breathing, over several consecutive hours.
Next, the final paragraph in this study sums up the whole purpose if this experiment. To give strength to the entire theory of source control and why so many people have fallen for it. Its source control...well...because it looks like its source control. I mean, look at it...its just obvious.
“In addition to providing an initial indication of the effectiveness of protective equipment, the visuals used in this study can help convey to the general public the rationale behind social-distancing guidelines and recommendations for using face masks.”
Hey, you know what would be more useful to the general public...is to know the contamination journey of the...actual...infectious particles, while we have this mask on all day.
(#6) Face coverings and mask to minimise droplet dispersion and aerosolisation: a video case study
Funding: by NHMRC Centre for Research Excellence (Grant Number 1107393), Integrated Systems for Epidemic Response. CRM is supported by a NHMRC Principal Research Fellowship, grant number 1 137 582.
Experiment Description: To provide visual evidence of the efficacy of face coverings we used an LED lighting system along with a high-speed camera (nac MEMRECAM HX-7s) to capture the light scattered by droplets and aerosols expelled during speaking, coughing and sneezing while wearing different types of masks We used a healthy volunteer without any respiratory infection and informed consent was obtained. The cough performed was voluntary and to induce a sneeze the subject used a tissue paper to stimulate the mucus membrane of the nasal cavity.
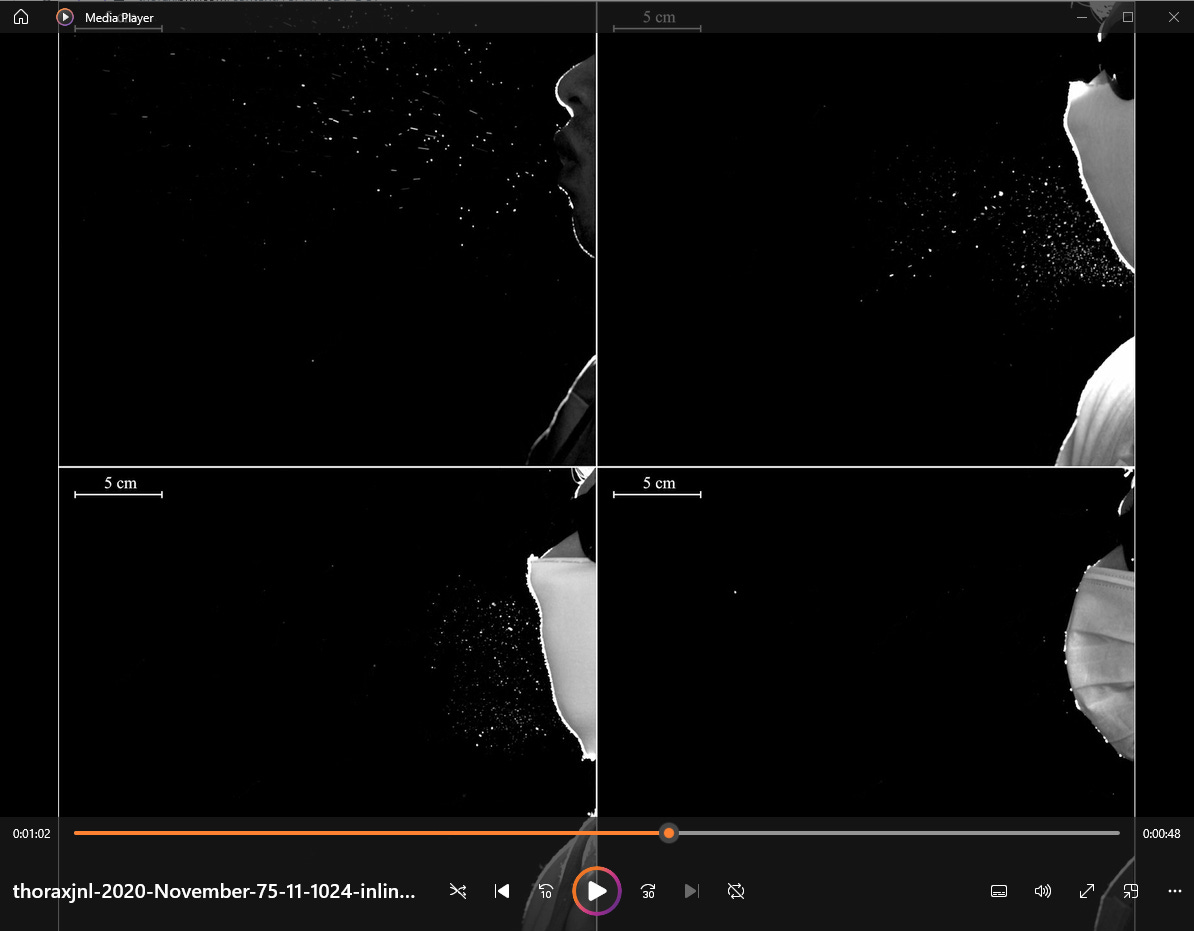
This is a frame from the video provided in the study. Notice how the camera was so obviously positioned to exclude the side gaps. This view remains constant throughout the video.
(#7) (from 2013) Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic?
Funding: Unspecified, but likely Public Health England (HPA), Porton Down Salisbury, UK.
Experiment Description: Several household materials were evaluated for the capacity to block bacterial and viral aerosols. 21 volunteers made their own face masks from cotton t-shirts; the masks were then tested for fit. The number of microorganisms isolated from coughs of healthy volunteers wearing their homemade mask, a surgical mask, or no mask was compared using several air-sampling techniques.
Some noteworthy excerpts;
“With 1 exception, all participants reported that their face mask was comfortable. However, the length of time each participant kept their mask on during testing was minimal (15 min), and with long-term wear, comfort might decrease.”
“The materials used in this published study were fresh and previously unworn. It is likely that materials conditioned with water vapor, to create a fabric similar to that which has been worn for a couple of hours, would show very different filtration efficiencies and pressure drops.”
Although the droplet sizes for both virus and bacteria were the same and affected the filter media in a similar manner, it was suggested that the viruses, after contact with the moisture on the filter, were released from their droplet containment, and driven onward by the flow of gas
...which is, the opposite of source control.
Conclusion (in its entirety)
“A protective mask may reduce the likelihood of infection, but it will not eliminate the risk, particularly when a disease has more than 1 route of transmission. Thus any mask, no matter how efficient at filtration or how good the seal, will have minimal effect if it is not used in conjunction with other preventative measures, such as isolation of infected cases, immunization, good respiratory etiquette, and regular hand hygiene. An improvised face mask should be viewed as the last possible alternative if a supply of commercial face masks is not available, irrespective of the disease against which it may be required for protection. Improvised homemade face masks may be used to help protect those who could potentially, for example, be at occupational risk from close or frequent contact with symptomatic patients. However, these masks would provide the wearers little protection from microorganisms from others persons who are infected with respiratory diseases. As a result, we would not recommend the use of homemade face masks as a method of reducing transmission of infection from aerosols.”
(#8) Respiratory virus shedding in exhaled breath and efficacy of face masks
Funding: General Research Fund of the University Grants Committee (grant no. 765811), the Health and Medical Research Fund (grant no. 13120592) and a commissioned grant of the Food and Health Bureau and the Theme-based Research Scheme (project no. T11-705/14-N) of the Research Grants Council of the Hong Kong SAR Government.
Experiment Description: 111 infected participants; coronavirus (17), influenza ( 43) rhinovirus (54). Cough samples over 30 minutes and also breathing samples, nasal and throat swab testing as well. Masks and no masks.used a bioaerosol collecting device, the Gesundheit-II to capture exhaled breath particles and differentiated them into two size fractions, where exhaled breath coarse particles >5 μm (respiratory droplets) were collected by impaction with a 5-μm slit inertial Teflon impactor and the remaining fine particles ≤5 μm (aerosols) were collected by condensation in buffer
Some noteworthy excerpts;
“Our findings indicate that surgical masks can efficaciously reduce the emission of influenza virus particles into the environment in respiratory droplets, but not in aerosols”
“Among the samples collected without a face mask, we found that the majority of participants with influenza virus and coronavirus infection did not shed detectable virus in respiratory droplets or aerosols, whereas for rhinovirus we detected virus in aerosols in 19 of 34 (56%) participants (compared to 4 of 10 (40%) for coronavirus and 8 of 23 (35%) for influenza). For those who did shed virus in respiratory droplets and aerosols, viral load in both tended to be low (Fig. 1). Given the high collection efficiency of the G-II (ref. 19) and given that each exhaled breath collection was conducted for 30 min, this might imply that prolonged close contact would be required for transmission to occur, even if transmission was primarily via aerosols, as has been described for rhinovirus colds”
(#9) Face coverings and respiratory tract droplet dispersion
Funding: L.B. is supported by the UK Engineering and Physical Sciences Research Council (EPSRC), grant no. EP/P017134/1. Ge.P. and Ga.P. are supported by the EPSRC grant EP/L016680/1, while E.M. by the EPSRC grant no. EP/S02431X/1. S.O.'s scholarship is funded by the Japan Student Services Organization. F.M. is supported by the European Commission (766840) and the EPSRC (EP/S001921/1 and EP/R035350/1), while P.D. is funded by the UK Biotechnology and Biological Sciences Research Council (BB/P013740/1).
Experiment Description: Several tests were done:
Manikin speech and cough simulator;”To ensure a significant number of landed particles could be detected prior to their evaporation, droplets were ejected from the manikin at a higher volume rate compared to a human being. Specifically, 20 min of speech test in the manikin corresponded to a subject counting from 1 to more than 10 000; 10 min of coughing tests modelled 60 000 human coughs.”
Laser imaging of droplets in flight: “We projected a thin laser sheet along the vertical plane through the mouth of the manikin and used a photographic camera to capture the light scattered by droplets passing within this plane”
Tests with human volunteers: “Six volunteers performed two rounds of coughing (1 min each) and speaking (3 min each) tasks, with and without a surgical mask. For each test, a glass slide was placed vertically, 5 cm in front of the individual's mouth. At the end of each experiment, the sample was imaged using widefield microscopy to count the droplets generated by the subject.”
Some noteworthy excerpts;
our data suggest that the wearing of masks can substantially reduce the probability of an infected person transmitting the virus. In this study, however, we focused only on the large respiratory droplets that land on a surface within a few seconds. According to the shadow imaging estimation of droplet size applied to the laser acquisition (electronic supplementary material, S4), these correspond to particles with diameters between 170 ± 7 and 590 ± 7 µm. Droplets as small as 26 ± 7 µm were detected with the laser but excluded from the analysis due to their non-ballistic trajectory. Other studies such as Fischer et al. [17], which focuses on in-flight droplets that include smaller droplets and aerosol, are likely to show a lower level of effectiveness depending on the fabric type. The aerosol is now widely accepted as a contributory route of SARS-CoV-2 virus transmission [5], and if this is later determined to be the main driver of infection, then our findings may overestimate the effectiveness of face coverings.
“Air was ejected at velocities and flow rates within the range of those observed from real individuals but droplets were ejected at a higher volume rate. Hence, the physical interaction between the droplets and the airflow jet was not correctly represented. However, this was necessary to ensure a high volume of particles and thus robust statistics, in a sufficiently short time frame to minimize evaporation of landed droplets and contamination with other particles in the environment.”
...that's a lot of words that mean “what we did has no connection to the real world”
“Furthermore, it was not possible to test if droplets escaped the mask and landed outside of the table. Viola et al. [14] showed that surgical and handmade masks can lead to lateral and backwards air jets. If a large droplet was carried by these jets, we would have not detected it. ”
So you only measured in the forward direction. Ok. Increasing the appearance of effectiveness of a device by NOT measuring the areas that would make the device look bad. Applying Hierarchy of Controls methodology we would call that “Elimination”
“In conclusion, these experiments demonstrate that both surgical and simple handmade masks such as a single-layer cotton mask can suppress the risk of direct person-to-person virus transmission through large droplet deposition. The data do not allow us to draw conclusions on the risks of virus transmission through aerosol inhalation. Assuming that SARS-CoV-2 virus transmission through aerosol is small compared to through large droplets, these results suggest that physical distancing can be reduced with the use of face coverings”
...yeah because PPE Controls are more powerful than Administrative Controls.....sarcasm.
(#10) Exhaled respiratory particles during singing and talking
Funding: This work was supported by Barbro Osher Pro Suecia Foundation, AFA insurance [grant numbers 180113, 200109] and the Swedish Research Council FORMAS [grant number 2017-00383].
Experiment Description: 12 singers, each executing various speaking loudness and various singing exercises in a chamber and apparatus used for measuring droplets. A high speed camera was used to capture droplet counts and behavior.
Some noteworthy excerpts;
When singing loud with a surgical mask, almost no droplets were detected with the camera.
Well heck, that sounds pretty good.
Singing generated more respiratory aerosol particles and droplets than talking. Exhaled aerosol particles and droplets increased with song loudness. The data also indicated that emissions might increase at high pitch. Wearing an ordinary surgical face mask reduced the amount of measured exhaled aerosol particles and droplets to levels comparable with normal talking. However, as surgical masks have a loose fit, some particles may have exited on the sides where we did not measure.
Nevermind.
(#11) (from 2019) Aerosol emission and superemission during human speech increase with voice loudness
Funding: National Institute of Allergy and Infectious Diseases of the National Institutes of Health (NIAID/NIH), grant R01 AI110703, and the NIEHS UC Davis Core Centre, grant P30-ES023513
Experiment Description: Droplet production and behavior; 48 participants engaged in some different speaking exercises; voiced /ɑ/ (the vowel sound in ‘saw’) for five seconds, followed by 15 seconds of nose breathing, repeated six times in succession. Then, Participants were asked to read aloud three times, at a comfortable pace, over approximately 2 minutes per reading. Also, Bilingual participants fluent in both English and either Spanish, Mandarin or Arabic red a short book chapter 3 times in each of their languages.
“To more closely represent normal conversational speech, the participants read aloud a short passage of text in English at varied loudness (quiet, intermediate, or loud). The reading experiment also was repeated in different languages to test whether choice of language matters; the results (Supplementary Fig. S5) confirmed the increasing trend between particle emission rate and amplitude, but exhibited no significant difference in the particle emission rate among the languages tested”
“Participants alternated four silent breathing patterns with vocalized speech at three amplitudes. For breathing measurements, the breathing patterns were designated as “nose” (both inhalation and exhalation through the nose), “mouth” (both inhalation and exhalation through the mouth), “deep-fast” (deep, slow inhalation for ~3 seconds through the nose, holding it for ~1 second, followed by fast exhalation through the mouth (~1 second)), and “fast-deep” (rapid inhalation through the nose (~1 second), holding it for ~1 second, followed by slow exhalation through the mouth for ~3 seconds). Each breathing experiment was performed over 2 minutes”
I have to wonder...does the CDC even understand the assignment here? Focusing on which words make more droplets....when what we really need to know is...where is the actual infectious contamination is going. We don't need experiments to tell us that droplets come out of our mouth when speaking, we already inherently knew this from our own observations as human beings.
We need science to tell us about things we can't see with our eyes.
There comes a point where it just seems like all of this is pomp and circumstance...a dog and pony show to make it look like something useful is being done. There really isn't a single study on the CDC list that gives us answers to anything that happens in universal public masking.
(#12)(from 2008) Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities
Funding: supported by the ARC Discovery Project DP0558410
Experiment Description: The aim of this research was to develop a system for investigating the size distribution of aerosols produced during expiratory activities and to investigate the short term
aging of these aerosols in terms of size distribution changes caused by the evaporation of the droplets water component. It involved breathing and speaking into a wind tunnel containing various instrumentation.
Some noteworthy excerpts;
“The study was fully scrutinised and cleared by QUT’s Human Research Ethics Committee. Fifteen volunteers were recruited on the basis of age (≤35 years), via a broadcast email invitation offering a small financial reward. They were instructed to self exclude if they were smokers, experiencing illness, asthma sufferers, had recently experienced expiratory problems or were likely to experience discomfort in confined spaces”
I've observed this “Ethics” stuff in many of the studies. I understand its a protocol step...but doesn't anyone else find it odd...even unscientific...that the results of a study conducted within the constraints of ethical parameters is allowed to be transferable to a general public afforded no such considerations?
To me this is why blanket “one size fits all” solutions should never be put into play...let alone forced on people. Especially when we are creating policy solutions from studies that are still on the low end of the Hierarchy of Evidence.
(#13)(from 2008) Speech can produce jet-like transport relevant to asymptomatic spreading of virus
Funding: NSF via the RAPID Grant CBET 2029370 (program manager is Ron Joslin) equipments donated by authors' various employers.
Experiment Description: Several tests of breathing and droplet behavior recorded with different methods of camera, heat sensory and lazers.
Some noteworthy excerpts;
“Phonetic characteristics of plosive sounds like “P” lead to enhanced directed transport”
“Our work will help better understand virus transmission in mammals, which can have catastrophic consequences in nature or affect the food supply. Building on the understanding of the fluid dynamics of viral and pathogen transmission we believe it will be possible to design potential mitigation strategies, in addition to masks and vague social distancing rules, and link to poorly understood issues of viral dose (39) to better manage societal interactions prior to introduction of a vaccine.”
Hmm...I think they’re imagining something like an HVAC system perhaps? LOL. Yes, engineering controls should be the dominant strategy.
(#14) Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2
Funding: NSF via the RAPID Grant CBET 2029370 (program manager is Ron Joslin) equipment donated by authors' various employers.
Experiment Description: airborne transmission simulator of infectious droplets/aerosols produced by mannequin simulated respiration and coughs and assessed the transmissibility of the infectious droplets/aerosols produced and the ability of various types of face masks to block the transmission. They used actual Covid virus in a sealed container with two heads facing each other 50cm apart. Performed various combinations of mask wearing. Respiration was exhaled continuously, simulating a mild cough at a flow speed of 2 m/s (2) for 20 min.
Some noteworthy excerpts;
In this study, infectious SARS-CoV-2 was exhaled as droplets/aerosols and mask efficacy was examined. To allow quantification, we conducted our studies by using a relatively high dose of virus, and under these conditions, it is possible that the protective capacity of the masks was exceeded. Although the efficiency of detecting infectious virus was reduced when the amount of exhaled virus was reduced, viral RNA was detected regardless of the type of mask used. These results indicate that it is difficult to completely block this virus even with a properly fitted N95 mask. However, it remains unknown whether the small amount of virus that was able to pass through the N95 masks would result in illness.”
It occurs to me that it would be prudent to know if there is an increase in the rate of leakage over time. For example in this case, Did the masks work well as source control for the first couple of minutes, and most of the contamination got through in the latter minutes? ...or was it a pretty consistent contamination over time?
In other words....if its “source control”....then how long is it source control? We already know N95's have a limited time use....just wondering how basic masks have unlimited capacity for perfection.
“When a mannequin exposed to the virus was equipped with various masks (cotton mask, surgical mask, or N95 mask), the uptake of the virus droplets/aerosols was reduced. A cotton mask led to an approximately 20% to 40% reduction in virus uptake compared to no mask (Fig. 2B). The N95 mask had the highest protective efficacy (approximately 80% to 90% reduction) of the various masks examined; however, infectious virus penetration was measurable even when the N95 mask was completely fitted to the face with adhesive tape”
Yeah those are decent numbers, but again this is perfect lab conditions that public policy is being made from. No real world parameters considered...and the behavior mechanic of the masks functionality is absent. PPE only works when it is used properly. Touching, adjusting wearing on chin or under nose, putting in pocket with phone, car seat, mirror etc. All of these things enable the continued journey of contamination. ( a.k.a. the “Behavior” mechanic of its functionality )
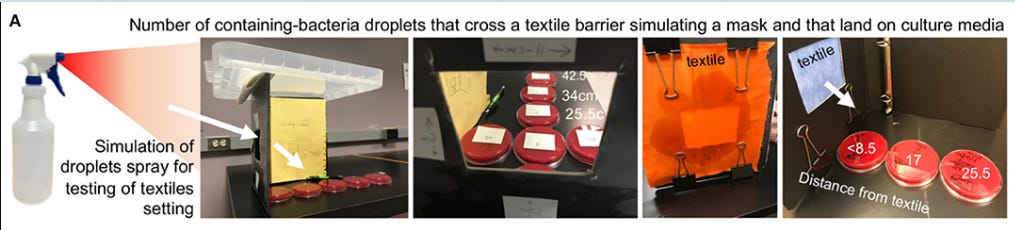
(#15) Textile Masks and Surface Covers—A Spray Simulation Method and a “Universal Droplet Reduction Model” Against Respiratory Pandemics
Funding: This study was conducted with discretionary funds allocated to AR-P and SI. AR-P received partial support from NIH via grants R21DK118373, entitled Identification of pathogenic bacteria in Crohn's disease, P30DK097948 NIH Silvio O. Conte Cleveland Digestive Diseases Research Core Center, and P01DK091222 (Germ-Free and Gut Microbiome Core) to FC and TP, Case Western Reserve University. AB received support via NIH F32.
Experiment Description: different fabrics were mounted in a frame and a solution was sprayed into them from a spray bottle. Petri dishes were laid on the other side to capture droplets that pierced the fabrics.
Some noteworthy excerpts;
“However, for asymptomatic individuals, not wearing masks in public could easily cause the spread of COVID-19. The prevention of “environmental droplet contamination” (EnvDC) from coughing/sneezing/speech is fundamental to reducing transmission. As an immediate solution to promote “public droplet safety,” we assessed household textiles to quantify their potential as effective environmental droplet barriers (EDBs).”
Typical of all of these experiments, is that no possibilities of environmental contamination are explored beyond just the droplets hitting the masks. What happens after that? No one knows because no study attempted to find out. Isn't another consideration that whatever infectious particles are left in the mask...are now being walked into other environments and exposing people to dangers they wouldn't have otherwise been exposed to had that person not brought their contaminated mask into it?
I imagine that those are the kinds of things industrial hygienists would wonder about and anticipate in their planning.
All textiles reduced the number of droplets reaching surfaces, restricting their dispersion to <30 cm, when used as single layers. When used as double-layers, textiles were as effective as medical mask/surgical-cloth materials, reducing droplet dispersion to <10 cm, and the area of circumferential contamination to ~0.3%. The synchronized implementation of EDBs as a “community droplet reduction solution” (i.e., face covers/scarfs/masks and surface covers) will reduce COVID-19 EnvDC and thus the risk of transmitting/acquiring COVID-19.
This statement clarifies that the authors have no understanding of the Hierarchy of Control. The behavior mechanic of PPE function is removed. What they are describing, is an engineering control.
Again we see the assumption being used as fact. That a mask reducing droplets equates to reducing infection. The focus here is on one mode of infection travel. There are several others, but they have been “eliminated” from the equation, so yes, the equation looks good.
Is there a point where the sum total of those other modes surpasses the one? If so, is it after a few minutes? 4 hours?...is there a point where any one alternative mode surpasses the one? If so, what are the conditions for, or time frame that these occur.
That is the underlying problem with the idea of “source control”. The same amount of contaminate is still in the immediate playing field. It is merely transferred to another surface area, and still on the move.
The question I'd like to see answered is...does a mask inhibit in any way via time or quantity, the other, more powerful controls in the area ( HVAC system) from being able to handle the contaminate in a timely manner. In other words...rather than just breathing into the room air and letting open windows, or HVAC do their thing...the contaminate is caught in the mask, and thus carried into another environment where such things don't exist to handle it.?
This is the kind of science that can answer the real life parameters we are navigating in universal public masking.
But what we get from the CDC is literally grade school science fair level stuff.
Here's more from the study...
“We then rationalized the potential impact of a “universal droplet reduction model” against pandemics, where the community act together to reduce the spatial range of EnvDC. Since it is unclear how many viral particles in droplets (virus/μm3) or surfaces (virus/cm2) are needed to acquire COVID-19, we assumed that any droplet on a surface area of 56.75 cm2 (an 8.5 cm diameter agar plate) renders a surface infective. Since textiles prevented droplets from reaching beyond a ~30 cm radius, we propose a working “droplet reduction model” to control COVID-19, where EDB-masks could reduce the “circumferential area of contamination” around each individual by 97.2% when used as single-layers”
Again a study describing masks as if they were an engineering control. They've removed the human element from their calculations.
The following, is an example of why it is CRITICALLY IMPORTANT to invest time in THOROUGH investigation of these studies. Doing so, gives you a clearer understanding of how authors guide the narrative of their study.
This paragraph from the Discussion section;
“NPIs are a critical component to achieve resolution. Although PPE, including masks, are scientifically-effective methods to prevent infectious disease transmission, the use of masks for the general public has not been encouraged by governments (5, 7), possibly because demand will deepen the current crisis of mask unavailability for medical staff, or alternatively, because the use of masks to prevent respiratory infections has been misleadingly deemed ineffective, despite earlier clinical studies indicating that masks could be beneficial in households during pandemics (35, 37, 38).”
a quick look at some referenced studies in support of claim that masks could be beneficial to households...
35; is about a family of six patients who traveled to Wuhan from Shenzhen between Dec 29, 2019 and Jan 4, 2020. This early study is more about transmission from human to human, but it is referenced in the mask space because of the observation that the 7 year old, who according to the mother was the most compliant about her mask, didn't get sick. But then again, it is also revealed in the data she was also around the rest of them the least.
37; conducted during the 2 winter seasons of 2006 and 2007. sick children ( and family) that presented to a caregiver were invited to participate. Mask use in household. The problem here is that everyone was also being treated with medications, room isolation etc.
38; This study has nothing to do with households or how well masks work. It was to determine the bioburdens of surgical masks in an operating room ( mask and hygiene contamination issues). While it does show that SM's ( surgical masks ) reducing growth in petri dishes, which is probably why the study was referenced.. it also measured and concluded that speaking with a mask causes more overall contamination to be created. It also showed that even when surgeons washing their face it does not reduce the amount of contamination build up on the mask surface during surgery.
(#16) Face Coverings, Aerosol Dispersion and Mitigation of Virus Transmission Risk
Funding: Unknown. Equipment and help with procedures were donated.
Experiment Description: We used a background oriented schlieren technique to investigate the airflow ejected by a person quietly and heavily breathing, and coughing. We tested the effectiveness of different face covers including FFP2 and FFP1 masks, a respirator, a surgical and a handmade mask, and two types of face shields. Finally, we simulated an aerosol generating procedure demonstrating the extent of aerosol dispersion.
Some noteworthy excerpts;
“Surgical and handmade masks, and face shields, generate significant backward leakage jets that have the potential to disperse virus-laden fluid particles by several metres. The handmade mask and the face shield opened at the bottom, showed an intense downward jet.”
Maybe we should call it “frontward only source control”
“For the FFP1 and FFP2 masks, which do not have the valve system, the airflow is pushed through the mask material and the front throughflow does not extend by more than 40 ± 2 cm for the FFP1 mask and 11 ± 2 cm for FFP2 mask. However, if these masks are not correctly fitted though, leaking jets are formed. These jets not only can travel significant distances (beyond the boundaries of our field of view), but are also only partially filtered because they do not flew through the mask fabric..”
I'd be curious to know whats happening to the particles that are making it through the mask material...is it going on the clothes now?, the floor? ...one place it probably isn't going....into the overhead HVAC system. Inquisitive minds would ask these questions.
“Surgical and handmade masks, and face shields, generate significant leakage jets that have the potential to disperse virus-laden fluid particles by several metres. The different nature of the masks and shields makes the direction of these jets difficult to predict, but the directionality of these jets should be a main design consideration for these covers. They all showed an intense backward airflow for heavy breathing and coughing conditions. It is important to be aware of this flow, to avoid a false sense of security that may arise when standing to the side of, or behind, a person wearing a surgical, or handmade mask, or shield. This is of relevance given the potential for some wearers of surgical masks to turn their face to the side when they cough, during face-to-face interactions with a colleague. In doing so, our data show that there is a risk that this backward jet is directed closer to a person standing in front of the wearer. Additionally, clinicians working around a patient, in the confined space around an intensive care bed or an operating table, are likely to be exposed to these side and backward leakage jets from surgical masks worn by colleagues.”
…but…but…source control.
(#17) Infectious Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Exhaled Aerosols and Efficacy of Masks During Early Mild Infection
Funding: This work was supported by Prometheus-UMD, sponsored by the Defense Advanced Research Projects Agency (DARPA) BTO under the auspices of Col. Matthew Hepburn through agreement N66001–18–2–4015. This work was also supported by the National Institute of Allergy and Infectious Diseases Centers of Excellence for Influenza Research and Surveillance (CEIRS) (contract number HHSN272201400008C) and the Centers for Disease Control and Prevention (CDC) (contract number 200-2020-09528). The findings and conclusions in this report are those of the authors and do not necessarily represent the official position or policy of these funding agencies and no official endorsement should be inferred. This work was also supported by a grant from the Bill & Melinda Gates Foundation, and a generous gift from The Flu Lab
Experiment Description: Recruited coronavirus (COVID-19) cases to give blood, saliva, mid-turbinate and fomite (phone) swabs, and 30-minute breath samples while vocalizing into a Gesundheit-II, with and without masks at up to 2 visits 2 days apart.
Some noteworthy excerpts;
Conclusions
SARS-CoV-2 is evolving toward more efficient aerosol generation and loose-fitting masks provide significant but only modest source control. Therefore, until vaccination rates are very high, continued layered controls and tight-fitting masks and respirators will be necessary.
“...provide significant but only modest source control” What does that even mean? Usually when you get side-eye statements like that its because word salad is being attempted.
“Viral RNA content of 30-minute breath aerosol samples was similar to the amount of RNA recovered from participants’ mobile phones”
“Loose-fitting face masks, including surgical masks and those in daily use by the study participants, produced significant, albeit modest, reductions in the amount of viral RNA in exhaled breath, supporting their use as source control. Consistent with previous studies of influenza, SARS-CoV-2 viral RNA was shed more abundantly in fine than coarse aerosol, and masks were more effective at blocking release of coarse aerosol”
“Overall, our results demonstrate that people with mild or asymptomatic SARS-CoV-2 infections released infectious aerosols in their exhaled breath. Face masks provided significant source control suggesting that community-wide masking even with loose-fitting masks can reduce viral aerosols in indoor air by half, making a significant contribution to reducing the spread of COVID-19. Our data also suggest that the virus is evolving toward more effective dissemination through aerosols and demonstrate that infectious virus can escape from loose-fitting masks.”
That paragraph seems to be contradictory. Keep in mind also, that this conclusive claim about the general public use of masks, was determined from a 30 minute perfect condition lab test.
(#18)(from 2010) Simple Respiratory Protection—Evaluation of the Filtration Performance of Cloth Masks and Common Fabric Materials Against 20–1000 nm Size Particles
Funding: National Institute for Occupational Safety and Health (CAN #927 Z1NT)
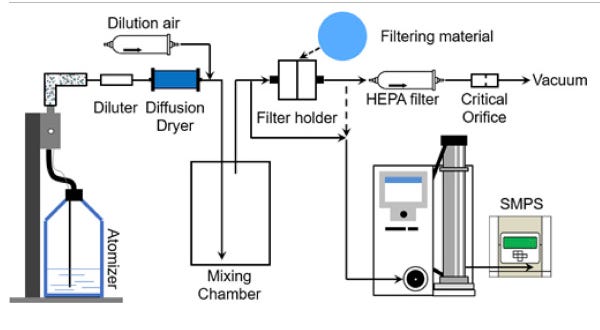
Experiment Description: simulated particle penetration tests on fabric samples, including N95 filter material. Using portacount equipment. 3 tests per material.
Some noteworthy excerpts;
Conclusion:
“Common fabric materials and cloth masks showed a wide variation in penetration values for polydisperse (40–90%) as well as monodisperse aerosol particles in the 20–1000 nm range (40–97%) at 5.5 cm s−1 face velocity. The penetration levels obtained for fabric materials against both polydisperse and monodisperse aerosols were much higher than the value for the control N95 respirator filter media but were in the range found for some surgical masks in previous studies. Penetrations of monodisperse aerosol particles slightly increased at 16.5 cm s−1 face velocity, while polydisperse aerosols showed no significant effect except one fabric mask with an increase. The penetration values obtained for common fabric materials indicate that only marginal respiratory protection can be expected for submicron particles taking into consideration face seal leakage.”
I think they were using this study to show that some protection is better than none. Which of course was floating around as a popular narrative point.
Again, my question is...for how long? At what point does that “some protection” get overrun by other variables working against the mask. Yeah we have no idea.
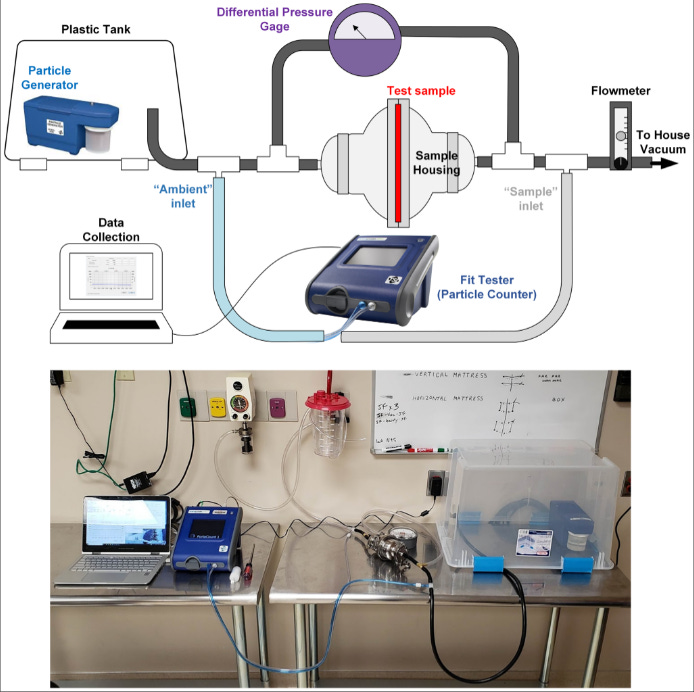
(#19) Measurement of filtration efficiencies of healthcare and consumer materials using modified respirator fit tester setup
Funding: The work described was supported by a Carle-Illinois College of Medicine Innovation Pathway Grant (medicine.illinois.edu). IB was supported by the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health (www.nibib.nih.gov/) under Award Number T32EB019944.
Experiment Description: A device was constructed to measure filtration on small pieces of materials.
( oh lookit that, a study about how mask work, that didn’t even use an actual mask )
Some noteworthy excerpts;
“Samples are cut to 91 mm circles to fit in the housing. Materials with a filtration efficiency greater than 40% are tested twice more using two additional samples.”
A tiny piece of cloth, in a sealed press...This has no relevancy to how masks work in public use, by just measuring only 1 of its 3 components of functionality. Design, and Behavior are absent. Plus, the material is set up in a way to achieve its best possible result. None of this advantage exists in public use.
“Three components determine the effectiveness of a face covering for transmission prevention: (1) the “fit factor,” which measures how well the mask seals to the face, (2) the filtration efficiency (FE), a material’s intrinsic ability to filter out particles in the air, and (3) the fluid resistance, a material’s ability to prevent penetration of fluids at pressures found in the human body. Medical respirators must meet metrics for all three, while surgical masks need only meet the latter two, with a lower threshold for filtration efficiency [16]. Though no standards currently exist for DIY masks, the same metrics are appropriate for comparative effectiveness. Other work has made inroads on mask fit and fluid resistance, but there is still substantial need for quantitative FE data to inform DIY mask construction [17–19]. The recent resurgence of universal mask usage globally has renewed interest in quantitative measurements and comparisons of materials for their design [20, 21].”
The authors are talking about masks as an engineering control.
They also don't realize that their metrics 2 and 3 are the same thing. The third metric is actually “Behavior”...the “instructions” for how the Design and the Materials are used...or put into action. Behavior...or worded differently....”Human Interaction”...is the primary reason PPE is at the bottom of the Hierarchy of Controls.
Elsewhere in the discussion...
“These data suggest that our setup provides a robust replication of NIOSH test standards. Furthermore, a recalled N95 from Tronex was measured at a FE of 92.95%, which can be compared with NIOSH measured FEs of 71–85% [48]. This comparison is challenging since these masks do not have printed manufacture dates or shelf lives and NIOSH results were from a single lot with unknown storage duration and conditions [48]. Additionally, our test sample intentionally minimized the presence of seams present in our smaller cross-sectional sample area, possibly contributing to a better observed performance. Similarly, the measured filtration efficiency of surgical masks, 74.36 ±4.54% correspond to values reported elsewhere [16].”
The NIOSH test standards it is referring to are specific to filtration by itself...not standards for the whole mask..which is what they are trying to infer…that its a reflection of the mask itself...but a reader wouldn't understand this subtle adjustment of wordplay unless they actually look deeper into the references.
It is also noteworthy that their surgical mask numbers are much higher than the results most other studies got with surgical masks. Of course that's because they are using a small section of the material and its sealed. Whereas other tests used the whole mask. The other thing they did here with their statement “correspond to values reported elsewhere [16]”...is that they cleverly referenced another study which also used cut-out sealed pieces of material.
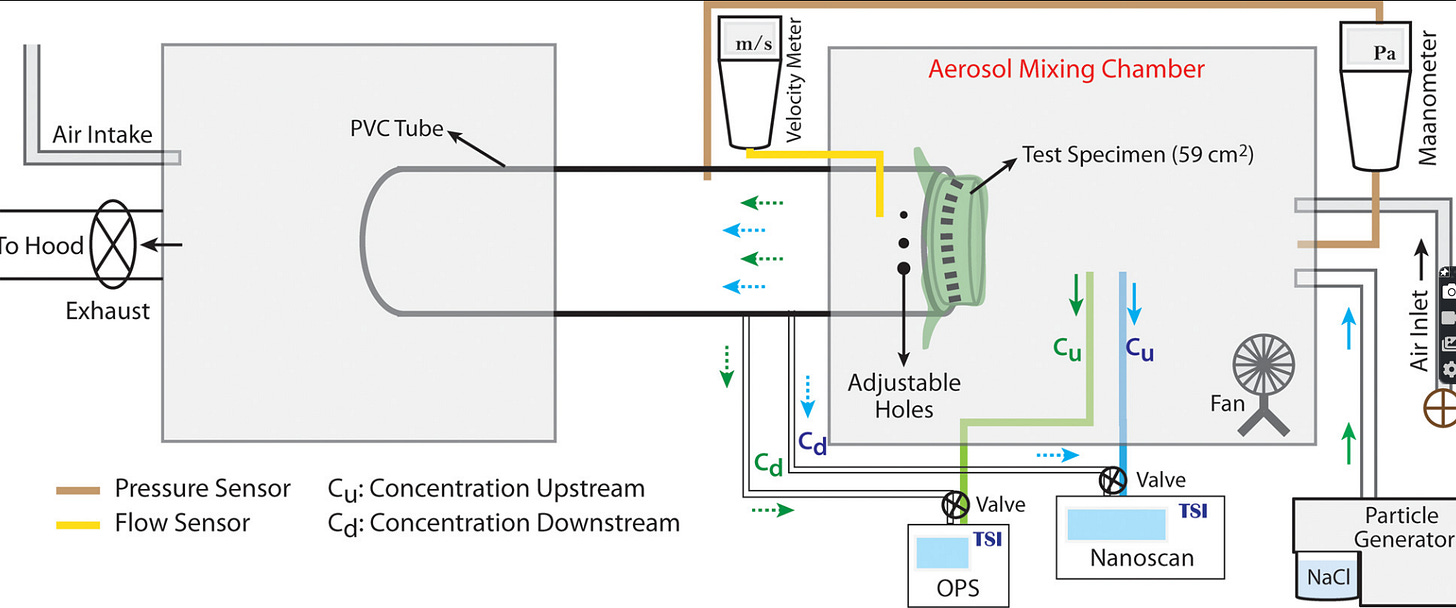
(#20) Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks
Funding: Department of Defense Vannevar Bush Fellowship Grant No. N00014-18-1-2869.
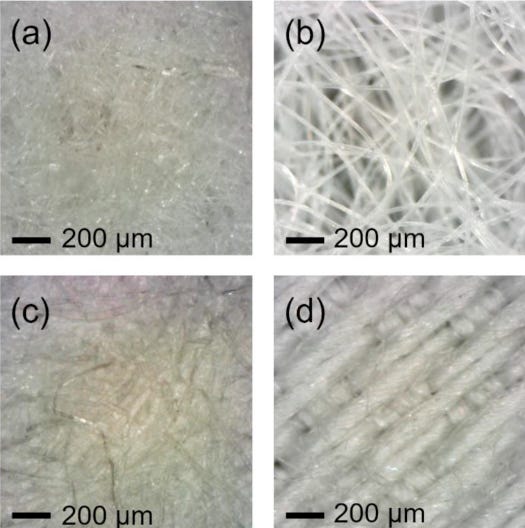
Experiment Description: A device was constructed to measure filtration on pieces of materials.
Some noteworthy excerpts;
In the illustration, notice that the source particles hit the sealed mask material BEFORE the gap holes. In real life its the other way around. The particles coming from the mouth have to deal with gaps first, mask second.
It is important to note that in the realistic situation of masks worn on the face without elastomeric gasket fittings (such as the commonly available cloth and surgical masks), the presence of gaps between the mask and the facial contours will result in “leakage” reducing the effectiveness of the masks. …..In our case, we have made a preliminary examination of this effect via the use of cross-drilled holes on the tube holding the mask material that represents leakage of air. For example, we compare the performance of the surgical mask and the cotton/silk hybrid sample with and without a hole that represents about ∼1% of the mask area.
Hmm, it seems that 1% gap isn't anywhere close to being realistic. I’ve seen the way people wear masks.
“the tests carried out with the 1% opening surprisingly resulted in significant drops in the mask efficiencies across the entire size range (60% drop in the >300 nm range). In this case, the two holes were ∼0.635 cm in diameter and the mask area was ∼59 cm2. Similar trends in efficiency drops are seen in the cotton/silk hybrid sample, as well. Hole size also had an influence on the filtration efficiency. In the case of an N95 mask, increasing hole size from 0.5 to 2% of the cloth sample area reduced the weighted average filtration efficiency from ∼60 to 50% for a particle of size <300 nm. It is unclear at this point whether specific aerodynamic effects exacerbate the “leakage” effects when simulated by holes. Its determination is outside the scope of this paper. However, our measurements at both the high flow (3.2 CFM) and low flow (1.2 CFM) rates show substantial drop in effectiveness when holes are present.”
Ok just think about that sentence in bold for a minute. Do you realize they are saying that they aren't sure whether their set up makes the leakage out of the tiny holes worse or better than the dynamics of realistic gaps. Their contraption is doing stuff and producing “numbers” but they have no idea about the how what or why of the numbers.
That statement renders the entire study dead in the water.
Regardless, with so much of it being a simulation, and the high level of uncertainty about it...there was a really obvious solution.
Use real masks and real people. Duh. That way you wouldn't have had to rely on drilled holes and guessing.
(#21) Ability of fabric face mask materials to filter ultrafine particles at coughing velocity
Funding: None Declared
Experiment Description: A device was constructed to test filtration of fabric samples. Particles were pushed for 3 minutes per test, at cough velocity. A fabric dampness test was included. by applying 7 mL of filtered water, the approximate amount of water exhaled by an adult during an hour of respiration, to the 5 cm2 section of the material.
Some noteworthy excerpts;
“Data from this study should be treated as preliminary”
“Ten readings were taken for each material, although one reading for the disposable High Efficiency Particulate Arrestance (HEPA) vacuum bag had to be later discarded due to a data transfer error. At least two different sections of each type of fabric were tested to ensure accurate representation of the material. Zero readings were taken on the particle testers regularly to ensure proper functioning”
Repurposing material for home-made face masks comes with its own risks. Consideration should be given to respiratory hazards which may arise from the material used to construct a home-made face mask. For example, concern has been expressed that certain HEPA vacuum bags include fibres which, if inhaled, can cause lung injury. Lint and fibres from fabric, when inhaled in large quantities, are known to contribute to multiple lung problems, including asthma, byssinosis and bronchitis. For this reason, we would caution those needing to create home-made face masks to ensure all materials are safe, non-toxic and lint-free. Fabrics which readily shed fibres may not be suited for face mask design. The risks associated with such materials are an important area of further study, as large numbers of people are currently creating, wearing, washing, distributing and selling home-made face masks. Further research should evaluate the ability of these materials and material combinations to filter specific viruses, pollutants and other harmful airborne particles.
It is our hope that this study can assist home sewers and makers to create the best face mask possible when standardised commercial personal protective equipment is unavailable.
Unfortunately the wish of these authors was never realized as none of their recommendations have ever been relayed to the public. But then again, the CDC hasn't relayed any of the important nuanced instructions from any of the other studies either.
The public was simply told they can make masks out of whatever. (shrug)
No potential collateral risks being introduced, were considered....that step was eliminated by simply saying “there's no downside to wearing masks”
and of course all of the employees at OSHA fell for it hook line and sinker.
(#22) Performance of fabrics for home-made masks against the spread of COVID-19 through droplets: A quantitative mechanistic study
Funding: unknown but various equipment contributions from authors, and this statement in the acknowledgements; Finally, we thank Dr. Faruque Ahmed of CDC for providing valuable guidance in conducting the research. ( he is a bigwig at the CDC, commanding a GS14 grade paygrade)
Experiment Description: a number of different types of tests were done using makeshift apparatus. Included high speed camera.
Some noteworthy excerpts;
Some particles can pass through the inter-fiber spaces (i.e. pores) as projectiles or be carried across by bulk fluid flow. Particles that are larger than the pores are simply blocked by straining or settling/caking. This is where the key distinction between established aerosol filtration models and blocking of large droplets emerges: While large solid particles will simply be blocked, a large droplet with sufficient momentum can squeeze through the pores of the fabric against shear stress and surface tension barriers
“We would like to stress that the efficiency values we report here are indicative of the ability of the fabric materials to block 100 nm-sized particles carried by droplets, and are not meant to reflect the net performance of a cloth facemask. The performance of a facemask would also depend on how it is worn, and how much air leaks through the gaps between the mask and face contours. Net efficiency of the facemask can be significantly lower than the efficiency of the fabric material itself, due to leakage through gaps”
You are probably starting to see a pattern in the observations from these studies...Particles escape through all edges of a mask.
So when you hear someone talking up source control and says “ you breath the droplets into the mask, it catches them, and the rest of the air goes out the sides
....you know now that it doesn’t work that way. At all.
(#24) Community Masks During the SARS-CoV-2 Pandemic: Filtration Efficacy and Air Resistance
Funding: No funding received
Experiment Description: We tested available community masks of major manufactures and determined the filtration efficacy using radioactive aerosol particles as well as air resistance with a vacuum measurement.
Some noteworthy excerpts;
“After a nebulization time of 20 seconds, the particles were homogeneously distributed and dried for 30 seconds using two fans installed inside the box (Fig. 1C). Water from the particles evaporates within a few seconds”
Ok...and then what happens??......pause......crickets.
The third-party and self-contamination risk increases with the working life of a protective mask(27,28); therefore, a regular change or a regular cleaning is mandatory. It is assumed that the moisture in the mask cloth as well as the contamination rate of the mask with airborne pathogens increases significantly with longer use of the masks. Blachere et al. called surgical masks and respirators a “personal bioaerosol sampler.”(29) Infectious particles from the mask surface could be further spread by contact or re-aerosolization causing self-infection or infection of others.(27–29)
a quick look at the references in that paragraph;
27, a 2019 study ignored by CDC.
“Respiratory pathogens on the outer surface of the used medical masks may result in self-contamination. The risk is higher with longer duration of mask use (> 6 h) and with higher rates of clinical contact. Protocols on duration of mask use should specify a maximum time of continuous use, and should consider guidance in high contact settings.”
28, a 2018 study ignored by CDC.
Results
The bacterial count on the surface of SMs increased with extended operating times; significant difference was found between the 4- to 6-hour and 0-hour groups (p < 0.05). When we analysed the bacterial counts from the same surgeon, a significant increase was noted in the 2-hours group. Moreover, the bacterial counts were significantly higher among the surgeons than the OR. Additionally, the bacterial count of the external surface of the second mask was significantly higher than that of the first one.
Conclusions
The source of bacterial contamination in SMs was the body surface of the surgeons rather than the OR environment. Moreover, we recommend that surgeons should change the mask after each operation, especially those beyond 2 hours. Double-layered SMs or those with excellent filtration function may also be a better alternative.
29, a 2018 study ignored by CDC. “This effort is part of a National Institute for Occupational Safety and Health 5-year multidisciplinary study to determine the routes of influenza transmission in healthcare settings.”
...but we're gonna listen to Fauci now so never mind any talk about contamination trails.
“Our results show that a HCW’s potential exposure to airborne influenza virus can be assessed in part through analysis of their SMs and N95 respirators, which can effectively serve as personal bioaerosol samplers.”
(#25) Testing of Commercial Masks and Respirators and Cotton Mask Insert Materials using SARS-CoV-2 Virion-Sized Particulates: Comparison of Ideal Aerosol Filtration Efficiency versus Fitted Filtration Efficiency
Funding: supported in part by the National Institute of Environmental Health Sciences of the National Institutes of Health under award no. R43ES030650.
Experiment Description: Mannequin headform fitted for particle production. Various masks were tested via portacount methods.
Some noteworthy excerpts;
“Fit clearly plays a critical role in the ability of a mask or respirator to protect its user from particulate inhalation. The as-received items did not show nearly the filtration efficiency when worn by the headform as was measured in base form despite apparent visual and tactile fit across the face of the headform, unless great effort was taken to seal the respirator–skin interface using adhesive.”
Proper fit is important, and air permeability of the filter material plays a role in where particles may travel in a loosely fitting mask, especially where smaller particulates are concerned which may more easily follow air vectors (9,10) around an imperfect fit.
There is a critical knowledge gap between understanding the dependencies on the relationship between filter material properties and mask fit. Indeed, one of the benchmark testing standards, ASTM F2299:2017 “Standard Test Method for Determining the Initial Efficiency of Materials Used in Medical Face Masks to Penetration by Particulates Using Latex Spheres”, calls out many of these limitations, including that it “does not assess the overall effectiveness of medical face masks in preventing the inward leakage of harmful particles” (11) This shortcoming has been demonstrated in the testing of medical masks before; (12) while the base material used to make common medical masks may demonstrate strong filtration efficiency according to established methods, the masks themselves often fail a basic quantitative fit test due to poor fit and resulting leakage. (13)
That emphasized sentence is telling us that the authors don't know how well lab results correlate to reality. Unfortunately these authors didn't do anything to answer that question here either.
(#26) Viral Filtration Efficiency of Fabric Masks Compared with Surgical and N95 Masks
Funding: This research received Flinders Medical Centre Foundation and Department of Innovation and Skills (Research, Commercialization and Startup Fund) funding to establish the mask testing apparatus
Experiment Description: A device was constructed to test materials filtration on whole masks
Some noteworthy excerpts;
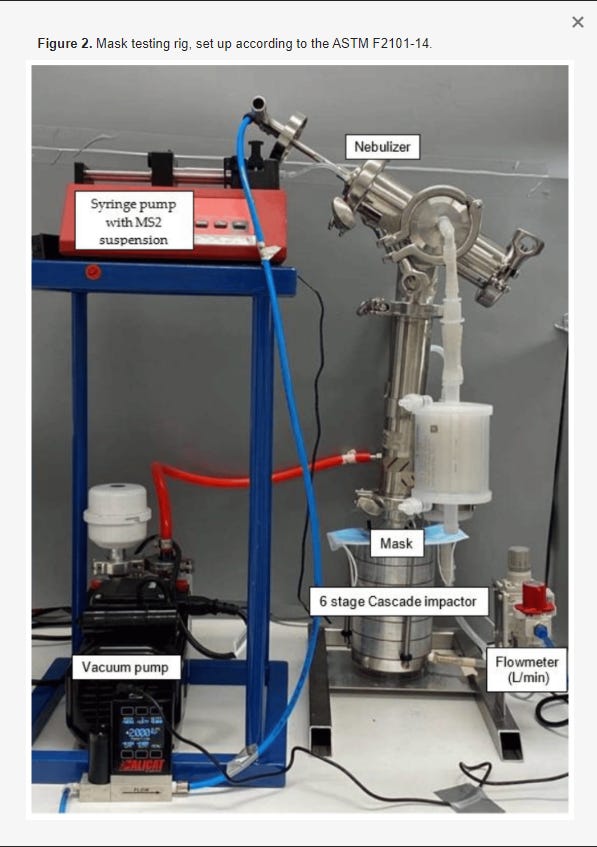
“Briefly, masks were challenged (see Figure 2 for challenge apparatus) with 200 µL of 8.3 × 105 PFU/mL MS2 viral aerosols in sterile water at a flow rate of 28.3 L/min, which is within the range of normal respiration and the limitations of the cascade impactor [18]. Masks were placed facing out to test their filter efficacy when used as a personal protection device. The pressure was maintained at 35 kPa and the challenge suspension was delivered for 1 min.”
“This study demonstrated that typically available fabric masks have at least a 50% viral filtration efficiency and this can be increased through the use of everyday items (vacuum cleaner bag and baby wipes) as an alternative to a disposable pocket filter or through designing fabric masks to have three layers of different fabrics. This research supports the use of fabric masks in community settings to prevent the spread of SARS-CoV-2.”
There is also the need for education campaigns aimed at informing individuals on how to wear fabric masks. This should include details on the best design and importance of good fit. There should also be advice on proper usage, including how to don and doff face masks, the importance of not touching masks to prevent self-contamination, and the need to wash masks in >60 °C water with soap or laundry detergent
We did see some of this, but it wasn't aggressive. The problem with telling people to do something correctly...doesn't mean they are actually doing it....which means you can't go ahead and calculate community results with the built in assumption that they did what you said simply because you told them to.....and this is exactly what happened with case studies.
I would assert that no one in the public did anything with masks correctly.....every day...all day. All through covid.
Sorry but that's just the reality of it....and we all know it.
(#27) Filtration performances of non-medical materials as candidates for manufacturing facemasks and respirators
Funding: This work is partly supported by the US National Science Foundation (NSF) 2027571
Experiment Description: A device built to measure filtration and particles. Materials properties also tested.
Some noteworthy excerpts;
“Compared to the more efficient commercialized medical and household air filters, all of the tested fabrics showed much lower filtration efficiencies, with below 60%. A scarf or bandana is not able to remove aerosols efficiently, even after multiple layers were stacked. For example, four layers of a scarf or a bandana only provide filtration efficiencies of 28.1% or 7.1% for 0.3 μm particles. These filtration efficiencies are not acceptable for removing airborne particles.”
However, once emitted, aerosols with different sizes may be subject to different evolution processes, such as evaporation, deposition, and decay of microorganisms, and the relationship between the number of viable viruses and aerosol size is still not well understood.
Evaporation? ..what contributes to evaporation? ….airflow.....what is the primary thing happening to masks all day long? ...breathing.....which is...”airflow”
As for particles with smaller sizes, the filtration efficiency will further decrease because the particle residence time is not long enough for particle collection via Brownian motion, which agrees with the previous studies
( for reference, the black line is 200.0 um. Covid is 000.2 um )
Brownian Motion is random bouncing around of particles from external forces and collisions of other particles. ...in other words...when the droplet is gone the virus travels.
(#28)(from 2008) Professional and Home-Made Face Masks Reduce Exposure to Respiratory Infections among the General Population
Funding: The study was funded by the Netherlands Ministry of Health, Welfare and Sports
Experiment Description: Three different experiments were undertaken to assess 1) short term protection for different types of masks worn during 10– 15 minutes by the same volunteer following a standardized protocol, 2) long-term protection of a specific mask worn continuously by a volunteer for 3 hours during regular activities, and 3) effectiveness of different types of mask in preventing outgoing transmission by a simulated infectious subject
Some noteworthy excerpts;
“Wearing of masks by caregivers might be more feasible and more effective, in particular where additional preventive measures are in place as well for caregivers.
...Yes and ALL of those measures have stronger effect than PPE ( Hierarchy of Controls )
Furthermore, we should bear in mind that this is an experimental study, with relatively small numbers of volunteers,
which limits the generalisability of some of our findings. E.g., for masks to have any impact during an actual pandemic, people may need to be wearing masks during several weeks with many shorter or longer mask-free periods. Furthermore, the PFs may be an over- or underestimation of the actual protection conferred. And although our simulated patient varied its breathing frequency, we have not assessed the impact of e.g. coughing or sneezing on outward transmission through a mask. A recent analysis than cities where some degree of transmission of the 1918 epidemic, noted that cities where strict interventions were implemented early on to prevent transmission, were overall worse-off urred early on [16]. Given the need for the population to acquire sufficient natural immunity over time, it can not be excluded that the amount of protection conferred by home made masks might sufficiently reduce viral exposure to impact on transmission during the early waves, while allowing people enough
exposure to start mounting an efficient immune response”
Interesting that in 2008 they understood about natural immunity and already had evidence that early mitigations didn't make a difference.
(#31) A laboratory-based study examining the properties of silk fabric to evaluate its potential as a protective barrier for personal protective equipment and as a functional material for face coverings during the COVID-19 pandemic
Funding: The authors received no specific funding for this work.
Experiment Description: simulated testing of several readily available materials for homemade masks. Special interest was taken in properties of silk.
Some noteworthy excerpts;
{droplet picture}
“Hydrophobicity is a measure of the ability of a material to repel small liquid droplets, thereby preventing the penetration and absorption of droplets, which are a vehicle for the transmission of the virus that causes COVID-19”
“We avoided any effects of kinetic energy on the contact angle formed by the droplet by ensuring the droplet was in contact with both the pipet tip and the surface of the material piece prior to final deposition”
That means they didn't drop it, they set it on the surface carefully. Because obviously that’s how it happens in real life when you cough and sneeze.
“The face coverings and surgical masks were positioned similarly as the face barriers to cover the index cards. The ear loops of the face coverings and surgical masks were put on the mannequin ears, and further held in place with pins (Fig 3). Initially, these face coverings were tested prior to any sterilization and stretching. After the initial trials, the face coverings were each sterilized using dry heat (70°C) [47] for 1-hour and then retested after a single sterilization and after five sterilizations. After each was sterilized, face coverings were worn for approximately 5-minutes by the same person (A.F.P.) and stretched (i.e., diagonally, horizontally, and vertically) to simulate wear-and-tear. The same face coverings and masks were used across all trials, and for each trial a mask or face covering was only sprayed once per technical replicate.”
“Currently, public health recommendations focus on cotton material for face coverings [17]. We found that cotton materials are hydrophilic, and readily allow droplets to rapidly penetrate and saturate the fabric like a sponge. Therefore, face coverings made out of these materials may quickly become reservoirs of virus and act as conduits for viral transmission when worn, even after a short time [5, 6, 30]. Face coverings made out of polyester face these same limitations, as we found it to be hydrophilic like cotton. Therefore, cloth and polyester face coverings appear to be more suitable for brief, one-time use.”
(#32) Strategies to minimize SARS-CoV-2 transmission in classroom settings: combined impacts of ventilation and mask effective filtration efficiency
Funding: unknown or none.
Experiment Description: Mannequins set up in a classroom setting to observe particle flow. Various measurements were taken, the study included math models, prediction and probability to reach some conclusions.
Note: this study was posted on the CDC while still in preprint form.
Some noteworthy excerpts;
All measurements were performed with the ELPI using the following procedure: (1) sample room air for 4 min without a mask, (2) install mask on the manikin, (3) sample room air through the mask on the manikin for 4 min after flow equilibrates (∼1 min), (4) remove mask from the manikin, and (5) sample room air for 4 min without a mask.
Measurements were performed with masks fit in a way that is representative of someone intent on effective use of the mask, that is, covering the nose and mouth completely and with the formable nose piece (if present) shaped to the manikin’s face. Additionally, an adjustable mask ear saver (Seljan Company, was used to allow the masks to be pulled tight to the manikin’s face
ahh...so your experiment was best case scenario....which is non existent in reality.
In reality, given the pressure drop across the mask filtration material it is expected that in normal mask wear a large fraction of the flow will go out the sides of the mask, significantly decreasing the filtration efficiency as worn, that is, the effective mask filtration efficiency. A simple estimate of the leakage velocity for a relatively low mask pressure drop of 20 Pa (v=(2ΔP)/ρ−−−−−−−−√ from the Bernoulli equation) gives a potential leakage velocity of 5.9 m/s, which for a 1 cm2 leakage area, would result in a leakage flow rate of 35 L/min (assuming a constant pressure drop). This flowrate is larger than the typical breathing flowrates associated with most activities (Adams 1993), indicating that if such a leakage path exists, most of the flow would follow that path and not go through the mask.
“The addition of knit cotton masks for all classroom occupants yielded a modest 15% reduction in aerosol conditional infection probability compared to the baseline with no masks. In comparison, the protective measure of increasing the ventilation rate from 1.34 ACH to 5.0 ACH resulted in almost a factor of two (1.87×) reduction, regardless of mask worn.”
Yes because HVAC is an engineering control.
This next paragraph alone negates the entire “source control” explanation you see on the promotional posters.
Mask aerosol leakage makes estimating infection probabilities using the Wells–Riley model highly uncertain when trying to take into account the effective mask filtration efficiency. We define EFE as the filtration efficiency of the mask as worn by the user. This is lower than the mask MFE which only considers the flow going through the mask material. In reality, given the pressure drop across the mask filtration material it is expected that in normal mask wear a large fraction of the flow will go out the sides of the mask, significantly decreasing the filtration efficiency as worn, that is, the effective mask filtration efficiency. A simple estimate of the leakage velocity for a relatively low mask pressure drop of 20 Pa (v=(2ΔP)/ρ−−−−−−−−√�=(2Δ�)/� from the Bernoulli equation) gives a potential leakage velocity of 5.9 m/s, which for a 1 cm2 leakage area, would result in a leakage flow rate of 35 L/min (assuming a constant pressure drop). This flowrate is larger than the typical breathing flowrates associated with most activities (Adams 1993), indicating that if such a leakage path exists, most of the flow would follow that path and not go through the mask.
Applying Bernoulli's principle to masks ( a fundamental principle of fluid and air dynamics) that are right next to your face (mouth) means that the air going out the smaller gaps of the mask will flow faster.
(#33) Quantitative Method for Comparative Assessment of Particle Removal Efficiency of Fabric Masks as Alternatives to Standard Surgical Masks for PPE
Funding: Funding for this work was provided by Northeastern University Office of the Provost through a COVID-19 Seed Grant. Advice, materials, tools, instruments, and time were donated or shared with us in order to carry out this project. A critical TSI PortaCount model 8028 was donated by Pfizer through the coordination of Luanne Kirwin, Sonya Ross, Rob Silk, John Price, and Michael Glover. Tools, advice, and expertise in conducting fit testing were generously provided by Gregory Lawless and Greg Olson, TSI Incorporated; Albert Thomas, the Massachusetts Department of Fire Services; George Mulholland, Department of Chemical and Biomolecular Engineering, University of Maryland; Marco Fernandez, National Institute of Standards and Technology; and John Price and Dan Meinsen, Environmental Health and Safety, Northeastern University. .
Experiment Description: standard portacount testing. Explore ways for public to increase efficiency
Some noteworthy excerpts;
Each mask test consisted of three 1-min runs while wearing the mask as designed (Figure 2A). In addition, the mask material was held against the face by adding a section of nylon stocking over the entire mask area following recommendations from Cooper et al.
9(Figure 2B) to simulate best possible fit and provide information on material filtration, and a single 1-min test was recorded in this configuration
“Given the limited time and current social distancing precautions, all tests were conducted while masks were being worn by the same subject, breathing normally, through the nose, with the mouth closed, while holding the head at a steady position”
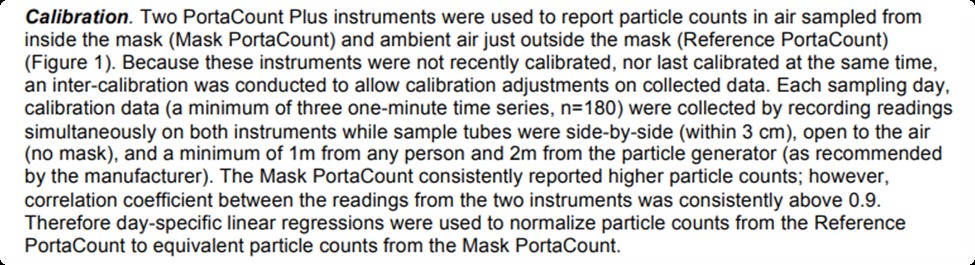
In addition, the portacounts were not calibrated before the experiments. (preprint published on MedRxiv April 24, 2020). The researchers did daily calculations as their version of calibration quality control. However, this introduces potential bias and error to the quality of the research.
The bigger problem is that this admission of non calibrations was omitted from the published study.
(#34) Evaluation of Cloth Masks and Modified Procedure Masks as Personal Protective Equipment for the Public During the COVID-19 Pandemic
Funding: Dr Clapp reported grants from the US Centers for Disease Control and Prevention (CDC) and UNC/US Environmental Protection Agency (EPA) Cooperative Agreement during the conduct of the study. Dr Sickbert-Bennett reported grants from CDC Epicenter (U54CK000483) during the conduct of the study. Dr Anderson reported grants from CDC Epicenter (U54CK000483) during the conduct of the study; grants from Agency for Healthcare Research and Quality, personal fees from UpToDate, and royalties for authorship outside the submitted work; and being the owner of Infection Control Education for Major Sports, LLC. Dr Weber reported grants from CDC during the conduct of the study. Dr Bennett reported grants from CDC during the conduct of the study and grants from the National Institutes of Health, US Department of Defense, US Food and Drug Administration, Cystic Fibrosis Foundation, and EPA outside the submitted work. This study was supported by the Duke-UNC Prevention Epicenter Program for Prevention of Healthcare-Associated Infections (U54CK000483) and a cooperative agreement between the University of North Carolina at Chapel Hill and the US Environmental Protection Agency (CR 83578501).
Experiment Description: portacount testing of common masks with and without alterations.
The total testing time for each mask was approximately 3 minutes.
The authors here are all doctors. What’s missing from this study? Risk analysis.
The irony is that this is the kind of thing that OSHA won’t touch.
“masks are technically not PPE”…oh ok….do the particles know this? It sure looks like real PPE, is being used as real PPE, doing the same exact job as real PPE, is dealing with the same pathogen as real PPE, covering the same hole as real PPE.
But somehow doesn’t have to deal with all the issues of real PPE.
Because magic. And yes magic is my real answer, until you can explain otherwise.
Some noteworthy excerpts;
Key Points
Question What are the fitted filtration efficiencies (FFEs) of consumer-grade masks, improvised face coverings, and modified procedure masks commonly used during the coronavirus disease 2019 (COVID-19) pandemic?
Findings In this comparative study of face covering FFEs, we observed that consumer-grade masks and improvised face coverings varied widely, ranging from 26.5% to 79.0% FFE. Modifications intended to enhance the fit of medical procedure masks improved FFE measurements from 38.5% (unmodified mask) to as much as 80.2%.
Meaning Simple modifications can improve the fit and filtration efficiency of medical procedure masks; however, the practical effectiveness of consumer-grade masks available to the public is, in many cases, comparable with or better than their non-N95 respirator medical mask counterparts.
Ok, so modifications bump the filtration numbers up, that’s great to hear. Ok, now can you tell me how much the lousy contamination behavior bumps it back down again?
No?….oh wait I forgot…the new science is that PPE is now an engineering control.
(#35) Maximizing Fit for Cloth and Medical Procedure Masks to Improve Performance and Reduce SARS-CoV-2 Transmission and Exposure, 2021
Funding: CDC
Experiment Description: Standard portacount tests on various materials and alterations.
Some noteworthy excerpts;
Here are the author affiliations...you would think it would add to the authority of the experiment, instead adds embarrassment to the institutions.
“CDC COVID-19 Emergency Response Team. 2Health Effects Laboratory Division, National Institute for Occupational Safety and Health, CDC.”
The Covid mask science as a whole, makes it clear that not only was it poorly done and low level ...but they didn't even understand the assignment to begin with.
We are talking about universal public masking and everything encountered within that playing field.
And yet not a single thing in that reality, found its way into the science projects....which were all just do-overs of existing studies, or existing processes anyway. Nothing new was introduced to the human race about masks.
“these experiments were conducted with one type of medical procedure mask and one type of cloth mask among the many choices that are commercially available and were intended to provide data about their relative performance in a controlled setting. The findings of these simulations should neither be generalized to the effectiveness of all medical procedure masks or cloths masks nor interpreted as being representative of the effectiveness of these masks when worn in real-world settings.”
“although use of double masking or knotting and tucking are two of many options that can optimize fit and enhance mask performance for source control and for wearer protection, double masking might impede breathing or obstruct peripheral vision for some wearers”
(#36) Fitted Filtration Efficiency of Double Masking During the COVID-19 Pandemic
Funding: Dr Bennett reported grants from the US Centers for Disease Control and Prevention and the US Environmental Protection Agency (EPA). No other disclosures were reported.
Funding/Support: This study was supported by the Duke University–University of North Carolina Prevention Epicenter Program for Prevention of Healthcare-Associated Infections (U54CK000483) through the US Centers for Disease Control and Prevention and a cooperative agreement between the University of North Carolina at Chapel Hill and the EPA (CR 83578501).
.
Experiment Description: portacount assessment of double masking. The fit test is 3 minutes long.
Some noteworthy excerpts;
Face-covering FFE was measured on 1 female volunteer (weight, 53 kg; height, 160 cm; head circumference, 56.0 cm) and 2 male volunteers with shaven faces (weight, 75 kg; height, 178 cm; head circumference, 58.5 cm; and weight, 76 kg; height, 175 cm; head circumference, 55.9 cm, respectively), as described previously.3,4 In brief, FFE corresponds to the concentration of particles behind the mask expressed as a percentage of the particle concentration in a sodium chloride particle–enriched chamber atmosphere [FFE% = 100 × (1 − behind the mask particle concentration/ambient particle concentration)] measured during a series of repeated movements of the torso, head, and facial muscles as outlined by the Occupational Safety and Health Administration Quantitative Fit Testing protocol.
Again, what happens to the contagious material once its in the mask...none of these experiments explores that question....All of this science is just assuming that the contaminated material just vanishes.
Here are some studies that the CDC put in their line-up, but then later removed.
Effectiveness of Common Fabrics to Block Aqueous Aerosols of Virus-like Nanoparticles
https://pubs.acs.org/doi/full/10.1021/acsnano.0c03972#
here they showed that even after 5 minutes of testing filtration, particles had made their way through the mask and onto the collection dish, and I posed the question of how much of the contaminated particles would eventually make their way through the mask after hours of continuous breathing.
Maybe all of them?
I know that the CDC was made aware of the shortcomings of this and other studies. The influence is unknown but the timing is suspect...
Shortly thereafter the CDC removed this study from their catalog of approved studies rather than address the question of long term particle filtration.
Another study that was quietly removed was;
Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2
https://onlinelibrary.wiley.com/doi/10.1002/jmv.25805
Yes..that is exactly what it looks like...one spray of droplets is being divided between 4 different masks simultaneously.
Aside from the horrendous methodology of squirting a simulated breath of droplets onto 4 separate material surfaces simultaneously. And it doesn't help when the supporting studies to your base argument, are exceptionally poor, or irrelevant.
For example, the study discusses RCT''s that support community masking....
Some randomized controlled trials (RCTs) did not support the efficacy of medical masks because medical masks could not reduce infection rates of some viral respiratory diseases.14, 15
Reference 14, is a mask experiment that exclusively used N95's
and reference 15 is an opinion piece written by an air purification company with something to sell.
The study also makes this statement...
Some other RCTs and many nonrandomized studies regarding the use of medical masks supported the notion that wearing medical masks could reduce infection risks of some viral respiratory diseases.8-14
Every one of those referenced studies are about N95's, or conflate the results of N95's and surgical masks in a hospital setting.
The biggest problem about trying to test hospital workers on the effectiveness of their PPE in keeping them from getting infected....is that they work in an environment with world class infection reducing technology and procedure all around them every hour of the workday.
And during times such as a pandemic...all of those other higher tiered controls are also being increased. Not just mask use.
To visualize it….in a hospital setting, everything on the hierarchy of controls is being increased
But ok sure....it was the masks….the weakest thing on the list, that did all the work.
This completes my summary of the CDC mask experiment studies.
yay, you did it. Thank You.
Now, pass this along to your spouses, friends, and most importantly your professional colleagues. It’s good to get the scientific discussions started…even if its at the water cooler.
The list of 90 can be found in this archived space here
Stay tuned for the “mask health studies” quick sheet.